Pregnancy
Pregnancy is a revolutionary experience for most women and men. Life gets a new dimension when you are expecting. It is one of the most precious and exciting periods in life.
At Cura you will meet the same midwife at the out-patient visits throughout the pregnancy, and together you will build a confidence that will give you strength and safety for the parenthood. We have long experience and high competence, and we can support you and your partner to get a secure and safe pregnancy.
Read more about our services under the flap Routine controls. Under the flap Ultrasonography overview you can read about the different ultrasound examinations performed during pregnancy.
Pregnancy is much of joy and expectation, but sometimes also unease and anxiety. We listen carefully and take your concerns seriously. Our doctors are up-dated and can offer you a meticolous medical care with easy access to ultrasonography when needed. Most often we can offer a quick and effective response to your need.
Today, the most important problems in obstetrics and neonatology are those children who are born too early, or are born too small (small-for-date). However, there are excellent possibilities to early identify such cases at risk, and timely take measures to prevent the problems.
In agreement with current evidence, we have made surveillance programs to estimate the risk of preterm birth, and to identify those babies who grow slowly in the womb. You can find more about these issues under the flaps Premature Prevention Program and Fetal growth.

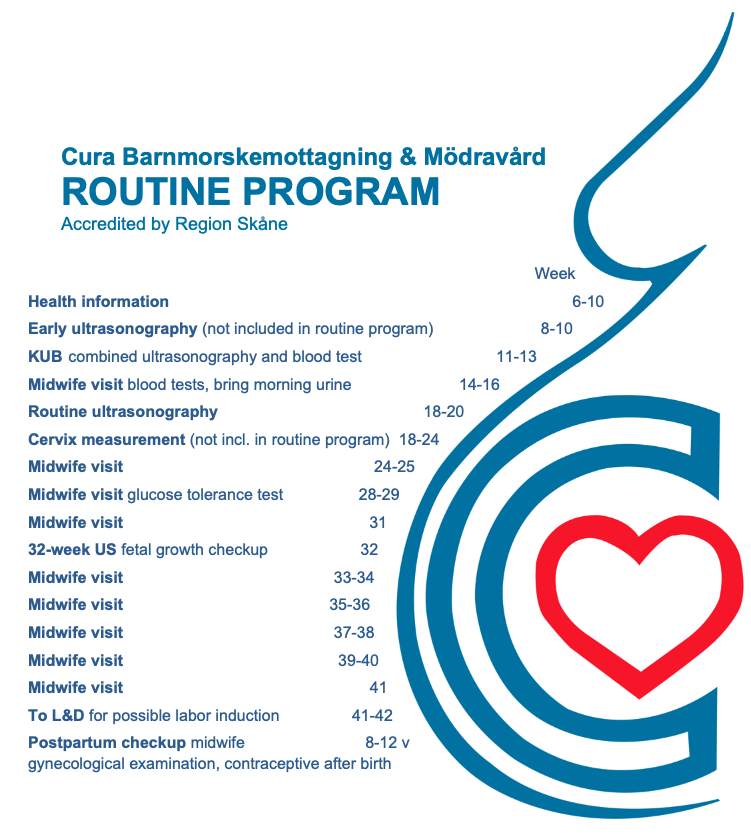
Routine program
Classes for parents-to-be
Classes for parents-to-be
Cura Barnmorskemottagning & Mödravård arranges information classes for women and their partners. The aim is to prepare you for the delivery and to strengthen your knowledge and security.
We talk about
- How you would know when labor starts.
- Who to call and when.
- What to bring to L&D.
- The role of your partner.
- What kinds of pain relief are available.
- Which complications could occur and how are they solved?
- Questions about breastfeeding.
- The first time with your baby.
The information is given in Swedish. Your midwife will tell you the time and place of the information.
Glucose tolerance test
Diabetes is a disease which increases with higher standards of living. The disease may occur at any age and sometimes it occurs during pregnancy. The risk is increased if relatives have the disease, and among certain groups of immigrants.
The reason why diabetes occurs during pregnancy is that there is a higher need of insulin to metabolize sugar. That is called insulin resistance. Women with a restricted ability to produce insulin might manage as long as they are not pregnant, but when pregnant the insulin production may become insufficient. Other women might have a previously undiscovered diabetes since before pregnancy.
It is of great importance for both mother and child that diabetes is discovered, because treatment should be started in time to avoid complications. In cases of gestational diabetes, the blood sugar levels usually returns to a normal level after birth. However, there is an increased risk of developing diabetes later in life.
By eating healthy food, staying fit and not overweight, it is probably possible to delay or even prevent from getting diabetes later in life.
The glucose tolerance test is routinely performed in gestational weeks 28-29. Those women who have a parent or a sibling with diabetes will have a test earlier in pregnancy. Sometimes the test is repeated also later in pregnancy.
In preparation for the test you should eat normally during three days preceding the test and stay fasting from 22.00 (10 PM) the day before the test. Fasting means that you should not eat or drink. You should also avoid excessive physical activity!
On the morning of the test you should arrive to the clinic no later than 08.00 in the morning (08 AM). A capillary blood test is taken by pricking the finger (fasting glucose). After that you are served a sugar solution to drink.
After that you will rest at the clinic for 2 hours, after which a second blood test is taken at 10 o’clock. It is wise to bring your breakfast to eat after the procedure!
In women having had a gastric-bypass operation, the glucose tolerance test will be performed at Specialistmödravården in Lund.

Ultrasonography overview
Early ultrasonography for viability
Many women want to have an ultrasonography performed already in gestational weeks 7-8 to ensure the pregnancy is normal. Such an examination is not included in the ordinary program for basmödravård, but we will organize it!
We perform a vaginal ultrasonography, which is much better than abdominal ultrasonography when very early in pregnancy. You can bring your smartphone and film the examination!
Contact us and book a time. You can find more information under the flap Early ultrasonography.
KUB – combined ultrasonography and blood tests
In the county of Skåne, all women are offered a free KUB (combined ultrasonography and blood test). At this procedure a blood sample is taken in gestational week 9+0 – 13+2 and an ultrasound examination is performed weeks 11+4 – 13+6 (preferably 12+0 – 13+2).
The aim of KUB is to identify fetuses with risk of having a redundant chromosome no. 21 (Trisomy 21, or Down syndrome), 13 or 18. However, it is important to be aware that KUB is only an estimation of risk and not a diagnosis of a redundant chromosome. If there is an increased risk of any trisomy, the woman is offered a diagnostic test.
A secondary aim of KUB is to date the pregnancy. Dating by KUB has a smaller error than dating by routine ultrasonography in weeks 18-20.
You can find more information under the flap KUB – combined ultrasonography and blood tests.
Routine ultrasonography
In Sweden all pregnant women are offered a free ultrasonography in gestational weeks 18-20. The aim of this routine ultrasonography is to reveal the number of fetuses, check for malformations, check the placental lie, and to date the pregnancy.
You can find more information under the flap Routine ultrasonography.
Cervix measurement
Measurement of the cervical length is performed to assess the risk of preterm delivery. The measurement is performed at 18-24 gestational weeks with an ultrasound transducer placed in the vagina (vaginal ultrasonography is more reliable than abdominal ultrasonography to measure cervix). In women having a previous late miscarriage or cervical conisation, the measurement is performed earlier. In some cases the measurement need to be repeated.
There is overwhelming scientific evidence that progesterone given vaginally to women with singleton pregnancy and a short cervix, can reduce the risk of preterm delivery in up to 40% and thereby also improve the health of the baby.
The International Federation of Gynecology and Obstetrics (the World organization of gynecologists) has recommended universal screening with cervical measurements in all pregnant women, but that has not yet been implemented in the routine care program in Skåne. However, we perform the measurements!
You can contact us and book an appointment for cervix measurement, and you can find more information under the flap Premature Prevention Program.
32-week ultrasonography
The 32-week ultrasonography aims to check the growth of the fetus. In this simple way, up to 70% more growth-restricted fetuses are detected compared when no 32-week ultrasonography is performed. Ultrasonography is a much better way to estimate the size and growth of the baby than our hands and a tape measures are.
If a slow growth of the baby is suspected, the controls and surveillance are intensified. It has been demonstrated that if a slow growth is detected already during pregnancy, the outcome for the baby will be better.
The routine 32-week ultrasonography was abandoned in Malmö-Lund a couple of years ago. However, at Cura Barnmorskemottagning & Mödravård we perform a routine 32-week ultrasonography if we think there is the slightest risk of slow fetal growth.
You can read more about ultrasonography for fetal growth under the flaps Blood flow measurements and Control for fetal growth and blood flow measurements.
Blood flow measurements
The blood flow measurements are performed with an ultrasound machine equipped to measure the blood flow velocity in blood vessels. In this way the resistance to flow (vascular resistance) in arteries supplying the placenta can be measured. An increased vascular resistance may indicate an impaired placental function.
Both arteries supplying the womb and the placenta are of importance to estimate the function of the placenta. If the vascular resistance is increased, there is an increased risk of slow growth of the fetus. The controls with ultrasonography for fetal growth and blood flow measurements must then be intensified. By repeated controls, it is possible to detect even small impairments.
Cura Barnmorskemottagning & Mödravård cooperates closely with Emma Ultraljudsklinik in surveillance of these pregnancies. In cases of impairments, or if planned delivery is discussed, the woman is always referred to the Skåne University Hospital.
You can read more under the flaps Blood flow measurements and Control of fetal growth and blood flow measurements.
Control of fetal growth and blood flow measurements
To estimate fetal growth, the head, abdomen and thigh are measured and the weight calculated. For correct weight estimation relative to the gestational age, dating by ultrasonography is necessary.
A poor fetal growth can be caught by the 32-week ultrasonography. A normal weight is between +22% and -22% above and below the mean weight, where 0% exactly corresponds to the mean weight.
A weight below -22% is called “suspected growth restriction”. Between two ultrasonography measurements, a fall of 10% or more is also called suspect growth restriction. Controls of fetal growth should not be performed in shorter intervals than 2 weeks, because there might be some percent measurement error and the fetus should have a chance to grow between the measurements.
Most often, fetal growth restriction is due to structural and functional lesions in the placenta. An impaired placental function can be detected by blood flow measurements, which is then a valuable complement to ultrasonography to follow the growth of a fetus. The resistance to flow is calculated, where an increased resistance indicates a risk of slow fetal growth.
At Cura Barnmorskemottagning & Mödravård we routinely perform a 32-week ultrasonography if there is the slightest risk of slow fetal growth. Blood flow measurements are performed when a risk of slow fetal growth is indicated.
Read more under the flaps Blood flow measurements and Control of fetal growth with blood flow measurements.

Early ultrasonography for viability
Ultrasonography for viability
The examination is performed as a vaginal ultrasonography by one of our doctors. By the vaginal approach the image quality is much better and the diagnostics are considerably safer than with an externally performed abdominal ultrasonography.
If you wish, you can bring your smartphone to videofilm the screen of the ultrasound machine!
What can we see at the examination?
- Gestational sac and embryo inside the womb
- Number of embryos
- Heart activity of the embryo (after about 6.5 weeks)
- The size of the embryo, measured as crown to rump length (CRL)
- Agreement between gestational age calculated as post menstrual date and by CRL
- To decide correct day for a KUB
- Yolk sac (acts as an early placenta)
- Missed abortion (no embryo, no heart activity) – a follow-up examination may be necessary
What can we not see at the examination?
- Gender of the embryo
- Site of the placenta in the womb
- Malformations
- Pregnancy outside the womb
The pregnancy is generally not dated by the early ultrasonography, but may be important for the surveillance program we decide for you.
The early ultrasonography is not included in the routine maternal health care services (basmödravård), but we perform the examination free of charge!
KUB – combined ultrasonography and blood tests
The aim of KUB is to identify fetuses with redundant chromosomes, but the examination is also important for determination of gestational age and for calculation of the expected date of delivery.
By KUB, a blood sample is drawn from the mother after 9 gestational weeks and an ultrasonography is performed at 11-13 weeks, preferably between 12+0 and 13+2. At this gestational age all fetuses have a small collection of fluid within the nape of the neck, and by ultrasonography the thickness of the fluid collection is measured. The fluid appears as a nuchal translucency. The fluid disappears later on, so the ultrasonography should be performed before 14 completed weeks.
In case a woman is uncertain about the date of her last menstrual period, or if she has irregular menstruations, it is worthwhile to have an early ultrasonography to settle the gestational age to ensure the booking for KUB is not too late.
Blood from the mother is sampled for analyses of beta-hCG (human chorionic gonadotropin) and PAPP-A (Pregnancy Associated Plasma Protein A), both of which are produced in the placenta. The blood test results are, together with the nuchal translucency thickness and maternal characteristics such as age, BMI, ethnicity, etc., used to calculate the risk of fetal chromosomal trisomies 21, 18 and 13.
The most common trisomies are Trisomy 21 (Down syndrome), Trisomy 13 and 18. It is then important to be aware, that KUB is not a diagnostic test, but just a test for calculation of risk. If the KUB result indicates an increased risk, further testing is necessary before a safe diagnosis can be settled.
If the risk is lower than 1 in 1000 (1/1000), there is a low risk that the fetus will have a trisomy and no further testing is needed.
If the risk is higher than 1/1000, further testing is offered: a risk between 1/51 and 1/1000 is an indication to take a maternal blood sample for NIPT (Non-Invasive Prenatal Testing), and at a risk of 1/50 or higher, invasive testing with amniocentesis (sampling of amniotic fluid) or chorionic villi sampling (CVS, tissues from the placenta) are offered.
By NIPT, a blood sample is drawn from the mother and the blood is analyzed for DNA fragments coming from the fetus. NIPT is however not accepted as a secure diagnostic test, so in case NIPT indicates an increased risk of trisomy, further testing with amniocentesis and CVS are offered. Which test to perform is dependent on the clinical situation and gestational age.
Amniocentesis and CVS are invasive methods, where samples are collected from the amniotic fluid or placenta through thin needles.
All prenatal diagnostics is voluntary and is performed in accordance with instructions from Region Skåne and Socialstyrelsen (Swedish National Board of Health and Welfare).
Cura Barnmorskemottagning & Mödravård co-operates with Emma Ultraljudsklinik, where KUB and possible further testings are performed. The staff has education and competence to perform prenatal diagnostics and will provide further information and support in case a finding is abnormal.
Patient informations in Swedish, English, Arabic and Soomaali are found if you google ”Fosterdiagnostik Skåne”.
The second aim of KUB is to determine the date of expected delivery. That date should be settled by ultrasonography at 11-22 weeks, where an early dating is best. Hence, dating by KUB is better than dating by the routine ultrasonography at 18-20 weeks. The date of expected delivery based on ultrasonography is called BPU (Sw. beräknad partus enligt ultraljud). BPU then corresponds to a gestational age of 39+6 weeks, i.e. 39 full weeks and 6 full days have passed of the pregnancy. A large difference between BPU and expected day of delivery calculated from the last menstrual period (when regular periods) could mean an increased risk of slower growth of the baby. At Cura Barnmorskemottagning & Mödravård we have therefore introduced a special surveillance program with extra ultrasonographies for determination of fetal growth and blood flow measurements if the difference is more than one week.
Routine ultrasonography
Routine ultrasonography is performed between gestational weeks 18 and 20. The examination is performed as an abdominal ultrasonography, i.e. the ultrasound transducer is placed on the belly. We can then
- See the number of babies.
- See the heart activity and body movements.
- Measure the size of the baby (head, abdomen, thigh) and estimate the gestational age and decide the estimated date of delivery (in Swedish BPU, beräknad partus enligt ultraljud).
- Examine the fetal anatomy and look for malformations.
- See the location of the placenta.
- Measure the amount of amniotic fluid.
Dating of pregnancy by ultrasonography is best performed between 11 and 22 weeks. An early dating has a smaller dating error than a later dating, and the KUB ultrasonography at 11-14 weeks is thus better for dating. In cases of more than one fetus, the dating is decided by measurements of the larger fetus. In cases where no ultrasonography has been performed at 11-22 weeks, an examination earlier than 11 weeks can be used for dating, whereas after 22 weeks there is a fairly large uncertainty. That is because in the same week some babies are larger and some smaller. Boy fetuses are larger than girl fetuses.
The benefits of the routine ultrasonography and secure dating are that
- The viability outside the womb can be estimated better: in Sweden a baby is viable at around 23 weeks.
- It is established when the pregnancy will be at full term (37+0 to 41+6 wks), postterm (from 42+0 wks), or preterm (22+0 to 36+6 wks).
- The proportion of postterm pregnancy will be halfed, from 9-10% when calculating postmenstrual age, to 4-4.5% when dating with ultrasonography.
- The number of labor inductions due to postterm, or postdate pregnancy, is reduced.
- The level of fetal surveillance and neonatal care at preterm deliveries can be optimized when knowing the precise gestational age.
The date of expected delivery is called BPU (Sw. beräknad partus enligt ultraljud). BPU then corresponds to a gestational age of 39+6 weeks, i.e. 39 full weeks and 6 full days have passed of the pregnancy. A large difference between BPU and expected day of delivery calculated from the last menstrual period (when regular periods) could mean an increased risk of slower growth of the baby. At Cura Barnmorskemottagning & Mödravård we have therefore introduced a special surveillance program with extra ultrasonographies for determination of fetal growth and blood flow measurements if the difference is more than one week.
Cervix measurement
The length of the cervix is measured with an ultrasound transducer placed in the vagina, to estimate the risk of preterm birth. The shorter cervix, the higher risk. Cervix should be measured by vaginal ultrasonography, because abdominal ultrasonography is not reliable for this purpose. Neither is a manual vaginal examination, because the length is most often underestimated.
The most important part of the cervix is the inner part, the internal opening. The inner opening is normally closed, but in rare cases it is widened. The fetal membranes (chorion and amnion) can then bulge into the cervix through the dilated inner opening, which results in a shorter part of the cervix being closed. This phenomenon, called funneling, can easily be seen by vaginal ultrasonography. It is always the closed part of the cervix that is measured. However, the cervix is dynamic and the depth and width of the funneling may vary, so it is necessary to look at the cervix for some minute.
The most extreme form of funneling is when the fetal membranes reach the external opening of the cervix. This is called cervical insufficiency. Sometimes the fetal membranes can even bulge into the vagina. Decades ago many doctors requested two or three late miscarriages before they were ready to settle the diagnosis cervical insufficiency, but that is an old-fashioned attitude. By vaginal ultrasonography we have learned the natural history of cervical insufficiency, i.e. that it starts with a funneling of the internal opening of the cervical canal. If we timely can diagnose a short cervix with or without funneling, we have good possibilities to prevent a late miscarriage or preterm birth.
The shape of the outer cervical opening is not as important as the inner opening is. The outer opening is often trumpet-shaped in women after giving birth.
It is however not only the length of the cervix that is important, but also other factors play role. You can read about that under the flap Premature Prevention Program.
When should the measurements be done?
The cervix is measured at a gestational age of 18-24 weeks. In women having had a late miscarriage or a conisation, the measurement may be performed already at 13-16 weeks. In many cases the measurement needs to be repeated. The examination is painless and does not increase the risk of miscarriage or preterm birth. No preparations are needed and the urinary bladder can preferably be empty.
What is a normal length of the cervix?
The cervical length is related to ethnicity, parity, age, height, and gestational age. It is therefore difficult to exactly define the normal length, but in the first trimester (before 14 weeks) the normal length is around 40 mm and after that the cervix shortens gradually with a few millimeters until term.
The shorter cervix, the higher the risk of preterm birth. A cervical length of 5 mm almost always results in birth before 32 weeks, but by increased length above that the risk rapidly decreases. There is no clearly defined limit for a short cervix, but after extensive research and discussions, the consensus of international scientists is that at 25 mm or shorter preventive measures should be taken.
Who should be examined with vaginal ultrasonography?
Pregnant women with known risk factors such as previous preterm birth or late miscarriage, twin pregnancy, malformation of the womb, conisation of the cervix, all run a higher risk of preterm birth. The risk of recurrence after a previous preterm birth is 30-50% and increases when more than one preterm birth. Other risk factors, though less serious, are low BMI, short interval between pregnancies, IVF pregnancy, smoking and drug abuse, physical and mental stress, and low/high age. These factors are more or less indications for a selective screening.
Pregnant women without risk factors run an increased risk of preterm birth if they have a short cervix. Several scientific studies have shown that universal screening is cost-effective in identifying those women. The International Federation of Gynecology and Obstetrics, which is the World association of gynecologists, has recommended universal screening with measurements of cervix, but that is not yet included in the routine program for mödravård in Region Skåne. However, we have such a program and you can read more under the flap Premature Prevention Program!
What is the treatment to prevent preterm birth?
There are two different types of treatment to prevent preterm birth, operation with a cervical cerclage (thread around the cervix) and progesterone medication. A third alternative, the Arabin pessary, has not yet been studied satisfactory to be clinically used.
There is today overwhelming evidence that vaginally administered progesterone is effective in women with a singleton pregnancy and a short cervix. The risk of preterm birth can be reduced by up to 40%, and thus also the risk of illness of the baby. In twin pregnancy the risk reduction is also significant, though not that much. Progesterone given as an injection is not effective.
A cerclage operation is an operation performed via the vaginal route where a thread is tied around the cervix. A planned cerclage operation is performed at 13-14 weeks, but an emergency (rescue) cerclage can be placed up to about 22 weeks. The thread is removed at 37 weeks. The indication for progesterone or cerclage is decided on an individual basis, but cerclage is indicated after a previous late miscarriage or extremely preterm birth, or when the cervix is very short with or without a funneling. When the cervix is open it is too late for progesterone, but a cerclage can be effective. Even in advanced cases, when the fetal membranes are bulging into the vagina, a cerclage may be effective.
You can find more about cervical insufficiency and the cerclage operation on https://www.sfog.se/media/64615/A.14.00.Olofsson.pdf
If you want to have a measurement of the cervix you can contact us (cost 300 SEK). You will find more information under the flap Premature Prevention Program.
32-week ultrasonography
The aim of the 32-week ultrasonography is to detect those fetuses who grow slowly, called “suspected growth restriction”. Dating by an early ultrasonography is then a prerequisite for a correct estimation of fetal growth. Ultrasonography is a much better way to estimate the size and growth of the baby than our hands and a tape measure are.
By the routine 32-week ultrasonography about 70% more fetuses with slow growth are detected, compared with if no ultrasonography is routinely performed. Hence, at clinics with a routine 32-week ultrasonography considerably more growth restricted fetuses are detected, which will improve the chance for the baby to be born healthy.
Previously a 32-week ultrasonography was included in the routine maternal care in Malmö-Lund, but that was ended a few years ago. However, at Cura Barnmorskemottagning & Mödravård we routinely perform a 32-week ultrasonography.
At the 32-week ultrasonography the head, abdomen and thigh of the fetus are measured and the weight estimated. For easy understanding and interpretation of the growth, the fetal weight is reported as deviation from the mean weight, expressed in percent. A weight exactly corresponding to the mean weight will then have a 0% weight deviation. The weight deviation is calculated for the very gestational day the measurement is performed. A normal weight deviation is then between +22% and -22%.
It is called “suspected growth restriction” if the estimated weight is -22% or below. However, all fetuses below -22% are not growth restricted, they might be genetically small because their parents are small. The mother’s size is then most important.
The normal reference curve is based on a Scandinavian population, which must be considered when women of different ethnicities are examined. A genetic smallness can be distinguished from a “true” growth restriction by repeated ultrasonography. A normal growth then indicates a genetic smallness. If the weight deviation falls with 10% or more between measurements it is suggestive of a slow growth and fetal growth restriction should be suspected.
A suspected growth restriction may appear also within the normal reference limits for fetal weight. Such a situation may appear if the fetus is programmed to be above the mean weight, but the ultrasonography shows it is below the mean weight. For that reason, we at Cura Barnmorskemottagning & Mödravård order blood flow measurement and ultrasonography already when the 32-week weight deviation is -11% or lower.
Two weeks must pass between two ultrasonography measurements for fetal growth, because there might be some percent measurement error and the fetus must have a chance to grow.
When a fetal growth restriction is suspected, there is an indication to perform a blood flow measurement. By doppler-ultrasonography the placental circulation is examined and the plan for the forthcoming surveillance can be optimized.
By the 32-week ultrasonography it is of course also possible to detect those fetuses at risk of growing too much, i.e. those who might become big. A follow-up ultrasonography at 36-37 weeks is then appropriate. However, there is a lack of clear guidelines how to handle pregnancies running a risk of “big baby”, that must be managed individually considering the past obstetric history and the size of the woman.
You can read more under the flaps Blood flow measurements and Control of fetal growth and blood flow measurements.
Blood flow measurements
An ultrasound machine equipped with doppler technique is used for measurement of blood flow in blood vessels of the womb and fetus. The doppler technique enables measurement of the velocity of moving targets, like when the velocity of cars is measured by radar. The velocity of the blood stream in blood vessels can be measured in the same way.
The machine can be adjusted to measure the velocity in a certain part of the vessel. With a precision of millimeters, the flow velocity can be measured in small and large blood vessels.
The blood flow resistance (vascular resistance) can be measured in arteries supplying an organ. When the resistance is increased, the flow during the relaxation phase of the heart (diastole) is diminished and the circulation in the organ is impaired. An increased vascular resistance therefore indicates an impaired function of the organ examined.
During pregnancy it is blood flows in the womb, placenta and fetus that are important. The blood flow of the womb is measured in arteries in the lower part of the womb, called the uterine arteries (uterus = womb).
There is one uterine artery on each side of the womb, located in the abdominal cavity close to the groin. However, the uterine arteries supply not only the placenta, but also other parts of the womb. The uterine blood flow measurements will thus not be a perfect measure of the circulation in the placenta. The uterine flow is then not a diagnosis of the placental function, but more of a prognosis of fetal growth in the future. In cases of an increased vascular resistance in the uterine arteries, there is risk of slow fetal growth. Depending on whether the uterine blood flow is affected or not, the intervals between ultrasonography and blood flow measurements to follow the fetal growth can be decided.
The uterine artery blood flow is thus a good guidance to how often controls should be performed. The indications to perform uterine blood flow measurements might be the patient’s history of diseases or previous problems during pregnancy, or when the 32-week ultrasonography alarms for suspected fetal growth restriction.
Since the uterine artery blood flow is more of a prognosis than a diagnosis, it is appropriate to perform the examination fairly early in pregnancy in women with a previous history of problems. At Cura Barnmorskemottagning & Mödravård, that means at 22-24 weeks and thereafter every second or fourth week, depending on blood flow and ultrasonography results.
The blood flows in the umbilical cord arteries represent the placental circulation considerably better than the uterine arteries do. An increased vascular resistance indicates a risk of a slower fetal growth. The cord blood flow is then a good guidance for management.
By repeated controls of fetal growth and blood flows, the fetal growth can be followed meticulously. It is then possible to be several steps ahead should any serious problems arise. It is then a key issue to identify those pregnancies where problems may occur. Here, the routine 32-week ultrasonography is an effective tool: around 70% more cases are identified compared with when no such examinations are performed routinely. Furthermore, when fetuses with slow growth are timely identified, the outcome for the baby is considerably improved. The 32-week ultrasonography was previously routine in Malmö and Lund, but was abandoned a few years ago. However, at Cura Barnmorskemottagning & Mödravård we perform a routine 32-week ultrasonography if we think there is the slightest risk of slow fetal growth.
By the ultrasound-doppler technique it is possible to measure blood flows also within the fetus, such as in the heart, brain, liver, and other organs. Such examinations are highly specific for certain problems and it is outside this text to explain their use.
You can read more under the flap Control of fetal growth and blood flow measurements.
Control of fetal growth and blood flow measurements
The fetal size and growth can be estimated by ultrasonographic meaurements of the head, abdomen and thigh of the fetus. It is then necessary that the pregnancy is correctly dated by an early ultrasonography.
The estimated weight of the baby is reported as percent deviation from the mean weight, calculated for the gestational day of measurement. If the weight exactly corresponds to the mean weight, the weight deviation is said to be 0%. In Sweden, a normal fetal weight is from 22% above the mean (+22%) to 22% below the mean (-22%).
If the weight is -22% or more below mean, it is called “suspected growth restriction”. However, a growth restriction can occur also within the normal reference ranges. A 10% limit for a fall in weight deviation has then been defined, i.e. if the fall in weight deviation is 10% or more between two measurements, there is suspected fetal growth restriction.
Controls of fetal growth should not be performed with shorter intervals than two weeks, because there might be some percent measurement error and the fetus should have the chance to grow between measurements.
However, some babies are genetically small because their mothers are small, or both parents are small. To distinguish the genetically small fetuses from growth restricted fetuses, blood flow measurements combined with repeated ultrasonographies are valuable.
In twin pregnancies it is expected that the babies will be smaller than in a singleton pregnancy. However, no reference curve for normal growth of twins is used, simply because there is no such Scandinavian curve that is good enough. Furthermore, it would be necessary to construct two curves, because the second twin is usually smaller than the first twin. Consequently, the same reference curve for normal fetal growth is used in twin and singleton pregnancies, and the same indications and limits used to perform extra controls of fetal growth and blood flow measurements. The growths of twins are routinely followed by repeated ultrasonographies. It is then important to know, that with reference to the singleton growth curve, twins in general show a slower growth than singletons after 30-32 weeks, and consequently they will show a more and more minus weight deviation.
You can find more about twins under the flap Twin pregnancy.
The vast majority of growth restrictions are caused by structural and functional lesions in the placenta. It may be disturbances from already when the placenta was established, or it may be infarctions developed later. With blood flow measurements the function of the placenta can be estimated.
Blood flow measurements are performed with an ultrasound technique based on the doppler principle. With doppler it is possible to measure the velocity of the blood stream in blood vessels. In that way, the resistance to flow (vascular resistance) can be calculated. An increased vascular resistance in the umbilical cord artery indicates an impaired placental function.
The blood flow is measured also in arteries supplying the womb, called uterine arteries, but these arteries are not only supplying the placenta but also the rest of the womb. As they are not placenta-specific, they are only a prognosis of the placental function, whereas the flow in the umbilical cord is a diagnosis of the placental function. The prognostic ability of uterine artery blood flow is to warn for a later developing fetal growth restriction.
It is logic to perform a prognostic test early in the course, and uterine artery blood flow measurements are performed in gestational weeks 22-24, before development of fetal growth restriction. The subsequent surveillance is to repeat the blood flow measurements and ultrasonography for fetal weight estimation and growth.
At Cura Barnmorskemottagning & Mödravård we routinely perform a 32-week ultrasonography if there is a risk of slow fetal growth. Blood flow measurements are performed when a risk of slow fetal growth is indicated.
Twin pregnancy

The rate of dizygotic (DZ, fraternal) twins relates to ethnicity. The rate in Sweden is slightly more than 1%, whereas it in Japan is 0.5% and in Nigeria 5%. The rater of monozygotic (MZ, identical) twins is similar Worldwide, about 0.4%. The rate increases by increased maternal age and is increased in some families. In IVF pregnancies the rate is related to the transfer of two embryos, but the rate of MZ twins is also increased. From the medical viewpoint it is important to know whether it is MZ or DZ twins.
The gestational sac has two fetal membranes, where the inner is called amnion and the outer chorion. DZ twins always have one of each, whereas MZ twins may have one of each, or a common chorion and different amnions, or both the chorion and amnion in common. In MZ twins it depends on the day of division into two of the original single embryo. An early division results in dichoriotic-diamniotic twins, some days later in monochoriotic-diamniotic twins, and a few days later in monochoriotic-monoamniotic twins. When dichoriotic-diamniotic there is a thicker membrane wall between the twins (4 membranes) than there is when monochoriotic-diamniotic twins (2 membranes).
At an early ultrasonography it is possible to see whether it is di- or monochoriotic twins. The optimal time is at 10-14 weeks. By ultrasonography the relation between the mucous membrane of the womb and the fetal membranes can be seen. It is also possible to see if the wall between the gestational sacs is thick or thin. A thin wall indicates MZ twins. It is important to see whether there are two separate or one single placenta.
At ultrasonography before 12 gestational weeks it is not rare to diagnose twins, but in about 20% it can be expected that one twin will vanish. Hence, if twins are diagnosed at an early gestational age it is wise to be somewhat restrictive in the information to friends and family.
At dating by ultrasonography it is from the size of the larger twin that the expected date of delivery is settled. Check-ups of fetal growths are performed at 24, 28, 32 and 36 weeks. The normal reference curve for growth is the same as the one used in singleton pregnancies, and it can then be expected that from around 30 weeks the weight deviation will be more and more minus because twins then grow slower than singletons. For simplicity, the same indications to perform extra growth controls and blood flow measurements are used in twin and singleton pregnancies. You can read more about that under the flap Control of fetal growth and blood flow measurements.
The main problem in twin pregnancy is preterm birth. The normal gestational age at delivery is slightly less than 37 weeks, so by definition a Little more than 50% of twins are born preterm. About 12% are born before 32 weeks. The earlier birth, the higher risk of problems of the newborn. Such problems could be difficulties in maintaining the body temperature, and problems with feeding and low blood sugar. More serious problems may affect the respiration and circulation.
Like in singletons pregnancy, a short cervix may indicate an increased risk of preterm delivery. The length of the cervix is easy to measure by vaginal ultrasonography and is performed at 18-24 weeks. Sometimes repeated measurements are necessary. Like in singleton pregnancy, a cervical length of 25 mm or shorter is defined as short. Research studies have shown, both in singleton and twin pregnancies, that if women with a short cervix is treated with progesterone vaginally the preterm delivery rate can be reduced, and thus also the risk of problems for the infant.
At Cura Barnmorskemottagning & Mödravård we have introduced a program for early detection of women with a short cervix and treatment with progesterone. You can read more under the flaps Measurement of cervix and Premature Prevention Program.
The twin in the lower part of the womb is called Twin 1, and the other Twin 2. The decision about mode of delivery depends on different factors, but in case there are no complications it is the lie of Twin 1 that guides whether a vaginal delivery or cesarean section should be planned for. If Twin 1 is in breech lie, a cesarean section is recommended. The lie of Twin 2 has no decisive importance for the choice of delivery mode. In uncomplicated cases where Twin 1 is in the head down position, there is no benefit in performing a cesarean section. In cases of preterm delivery before 33 weeks the choice is usually cesarean section.
In cases of uncomplicated dichoriotic-diamniotic twin pregnancy, with head down of Twin 1, induction of labor is considered at 38-39 weeks. It is generally accepted that the risks are lowest at that gestational age. In cases of complications, and when other types of twins, other considerations about time and type of interventions are made.
The activity in the delivery room is higher with twins than with singletons. There is a need to check the position of Twin 2, guide Twin 2 to a longitudinal lie, put on and off the infusion for stimulation of contractions, and to take care of two newborns.
Premature Prevention Program

Summary
There are today convincing scientific evidence that vaginally applied progesterone given to pregnant women with singleton pregnancy and a short uterine cervix can reduce the risk of a too early delivery by up to 40%, and hence also the risk of illness of the child. There is no evidence that the medication is harmful for mother or child. A universal screening with measurement of cervix in all pregnant women and prescription of vaginal progesterone to those with a short cervix may reduce the rate of preterm birth in the population and then also the morbidity and mortality among the children.
Introduction
Preterm delivery means that the baby is born before 37 full gestational weeks. The earlier birth, the higher risk of problems of the newborn. Such problems could be difficulties in maintaining the body temperature, and problems with feeding and low blood sugar. More serious problems may affect the respiration and circulation. The Premature Prevention Program aims to decrease the rate of preterm birth and the risks for the child.
There are multiple possible reasons for a preterm birth, such as infection, impaired function of the placenta with slow fetal growth, high blood pressure, high or low age, stress, conisation of the cervix, or overextended uterus as with twins. In many cases no reason is found, but in other cases the cause is a short cervix. A cervix of 25 mm or shorter (≤25 mm) increases the risk of preterm delivery 6-fold.
Recent research has shown that vaginally applied progesterone may prevent births before 33 weeks by 38% in women with a short cervix. The treatment is daily and should be maintained up to at least 34 weeks. No adverse effects on mother or child have been found. An operation with cerclage (a thread applied around the cervix) may be chosen in certain cases. You can find more about the cerclage operation on https://www.sfog.se/media/64615/A.14.00.Olofsson.pdf
Pregnant women with known risk factors such as a previous preterm birth or late miscarriage, twins, malformation of the uterus, or conisation of the cervix, run an increased risk of preterm birth. After a previous preterm birth, the recurrence rate is 30-50% and it increases further by additional numbers of preterm births. Other risk factors, though less serious, are low BMI, short interval between pregnancies, IVF pregnancy, smoking and drug abuse, physical and mental stress, and low/high age. These factors are more or less indications for a selective screening.
Pregnant women without risk factors run an increased risk of preterm birth if they have a short cervix. By international consensus, the limit was set to 25 mm. Several scientific studies have shown that universal screening is cost-effective in identifying women with a cervix ≤25 mm. The International Federation of Gynecology and Obstetrics, which is the World association of gynecologists, has recommended universal screening with measurements of cervix, but that is not yet included in the routine program for mödravård in Region Skåne. However, the Premature Prevention Program is such a program!
Measurement of cervix
The cervix is measured at 18-24 weeks by a ultrasound transducer placed in the vagina. Women with a previous conisation or late miscarriage should have the examination earlier. Measurements of cervix by abdominal ultrasonography are not reliable. In some cases repeated measurements are needed. The examination causes no pain or increased risk of miscarriage or preterm delivery. No preparations are needed.
Management and guidelines
The Premature Prevention Program is in accordance with guidelines from The Fetal Medicine Foundation (UK), The Society for Maternal-Fetal Medicine (USA), The American Congress of Obstetricians and Gynecologists (USA), The National Institute for Health and Care Excellence (UK), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists, and The Intentational Federation of Gynecology and Obstetrics. Swedish national guidelines are lacking.
The guidelines means that (A) women with a previous late miscarriage or spontaneous preterm birth are treated with progesterone irrespective of the length of cervix, whereas (B) women with or without risk factors are screened with measurements of cervix and treated with vaginal progesterone if the cervical length is ≤25 mm. Controls with repeated measurements are then performed to follow the course. At 18 weeks 0.9% of women have a cervix ≤25 mm, and at 24 weeks 4.2%. There is no difference in management between first-time pregnant women and women with previous births.
Treatment
Progesterone is an endogenous hormone with effects on the womb, cervix and fetal membranes. A low progesterone level could accelerate the maturity of the cervix and loss of the mucus plug, thus increasing the risk of preterm birth. A short cervix may be a sign of a too early maturation. The treatment is daily application of progesterone in the vagina. The treatment is just as effective in first-time pregnant women as in women having previous births.
Most gynecological societies recommend treatment until gestational week 33+6, but since 72% of all preterm births occur after that, the recommendation can be questioned. Some societies then recommend treatment until 36+6 weeks.
Sometimes there is an indication to place a cerclage. Cerclage is an operation where a thread is placed and tied around the cervix to close the cervical canal. The indication for cerclage is decided from case to case, but in Sweden the operation is rarely performed after 22 weeks.
The mean gestational age at birth is for twins slightly less than 37 weeks, i.e. preterm birth occurs in a little more than 50%. A short cervix is also in twin pregnancy a sign of a too early maturation of the cervix and the same guidelines as in singleton pregnancies are valid.
Treatment results
In a meta-analysis performed by leading international researchers, vaginal progesterone was administered to 498 women and placebo (“sugar pills”) to 476 women with a cervix ≤25 mm. Progesterone thus reduced the risk of birth before 33 weeks by 38% (from 22.5% to 13.9%). The corresponding reduction for births before 36 weeks was 20%. In addition, the risk of serious complications in the infant was reduced with 41%.
Universal screening was introduced at many clinics in the USA and Australia some years ago, resulting in a decline in preterm births. A general decline of preterm births has been seen in the USA during the last 7 years, which is credited the increased use of vaginal progesterone in women with a short cervix.
Managements of pregnancies at increased risk of complications are at present not included in the accreditation agreement of basic maternal health care services (Sw. basmödravård) with Region Skåne, but should be managed at the Specialistmödravården at the Skåne University Hospital. As an alternative for women at risk of preterm delivery, participation in the Premature Prevention Program is offered at a price of 300 kronor per visit.
Contact us if you want to participate in the program.
Labor & delivery
It is often difficult to decide whether labor has started or if it is contractions during the latency phase. Labor contractions are more regular with back pain and pain towards the groins. The latency phase may cause great discomfort but the pain is usually not as strong. By definition, a woman is not in labor until the contractions are regular and some effacement and opening of the cervix have occurred.
A loss of the mucus plug may occur without any contractions and is alone not a true sign of start of labor. There is no need to contact the labor & delivery ward because of loss of the mucus plug! Rupture of the membranes with watery discharge or flooding may occur without any contractions, but it is more common that the membranes rupture during labor. A small bloody show may indicate that labor has started.
When is it time to contact the maternity unit at the hospital?
- When you have 3-4 regular contractions per 10 minutes.
- When rupture of the membranes.
- When significant bleeding.
If regular contractions occur before 37 gestational weeks there is always a reason to contact the hospital. Another reason is strong and persistent pains. You may also contact the hospital if you have worry and anxiety you cannot master.
Many women stay at home in the beginning of labor. You can call the Skåne University Hospital in Malmö or Lund, phone number 0771-111 888, and talk to a midwife.
Before you leave for the hospital, it is important to call and tell that you are coming, and to make sure there is a room for you in the L&D.
You can chose yourself at which maternity unit within Skåne you want to give birth. Bring you Birth Plan Letter where you have written down you expectations and wishes. The staff will do their best to fulfill your wishes.
Postpartum checkup
It is important to attend the checkup visit with your midwife after birth. The midwife checks the healing and you have possibilities to ask about your course of labor and delivery. At the postpartum checkup you can also get a contraceptive prescribed.
You have to book the visit yourself. The appropriate time is 8-12 weeks after birth. Call 040-98 70 70 or send an email.
